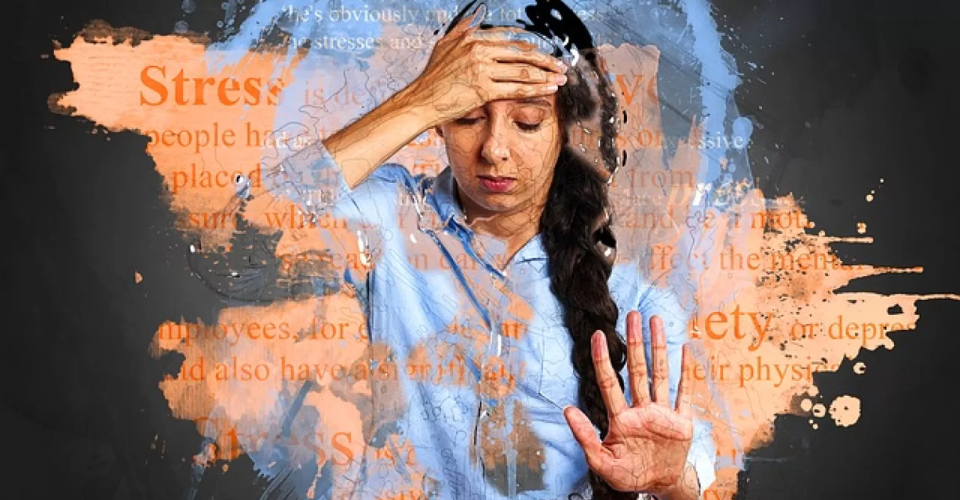
In the wake of the COVID-19 pandemic, the United States is grappling with the psychological aftermath of a collective trauma, according to a new survey conducted by the American Psychological Association (APA).
Despite the appearance of a return to normalcy, psychologists warn that the post-traumatic effects on mental and physical health are more substantial than meets the eye.
The long-term stress endured since the pandemic’s onset has taken a significant toll on well-being, with a notable increase in reported mental health conditions and chronic illnesses.
Survey To Understand The Collective Trauma And Stress
These findings come from the “Stress in America™ 2023” survey, which polled over 3,000 U.S. adults aged 18 and older, conducted by The Harris Poll on behalf of the APA.
The survey’s results reveal that individuals aged 35 to 44 experienced the most significant rise in chronic health conditions post-pandemic, with 58% reporting such conditions in 2023 compared to 48% in 2019.
This same age group also saw the highest increase in mental health diagnoses, with 45% reporting a mental illness in 2023, up from 31% in 2019. Adults aged 18 to 34 still had the highest rate of mental illnesses, with 50% reporting such conditions in 2023. Adults aged 35 to 44 were also more likely to attribute significant stress to money (77% vs. 65%) and the economy (74% vs. 51%) in 2023 compared to 2019.
“The COVID-19 pandemic created a collective experience among Americans. While the early pandemic lockdowns may seem like the distant past, the aftermath remains,” stated Arthur C. Evans Jr., PhD, APA’s chief executive officer.
“We cannot ignore the fact that we have been significantly changed by the loss of more than one million Americans, as well as the shift in our workplaces, school systems, and culture at large. To move toward post-traumatic growth, we must first identify and understand the psychological wounds that remain.”
Interestingly, many respondents maintained positive perceptions of their physical health despite being diagnosed with chronic conditions. Over 81% of adults rated their physical health as good, very good, or excellent. However, 66% of adults acknowledged having been informed by a healthcare provider about a chronic illness.
Similarly, 81% of respondents reported good, very good, or excellent mental health, yet more than a third (37%) stated they had a diagnosed mental health condition. This is a 5 percentage point increase from pre-pandemic levels in 2019 (32%).
The majority of adults downplayed their stress, with 67% believing that their problems aren’t “bad enough” to warrant stress compared to others who may have it worse. When asked why they don’t seek treatment, the top reasons included a belief that therapy doesn’t work (40%), a lack of time (39%), or insufficient insurance coverage (37%).
Nevertheless, 47% expressed a desire for someone to help them manage their stress, while 62% admitted to not discussing their stress with others to avoid burdening them.
The survey found that nearly a quarter of adults (24%) rated their average stress level between eight and 10 on a scale of one to 10, where one signifies little to no stress, and 10 indicates a significant amount of stress.
This is an increase from 19% in 2019, before the pandemic. The rise in stress was consistent across all age groups except those aged 65 and older. Among individuals aged 18 to 34, 34% reported high stress in 2023, up 8 percentage points from 2019. For those aged 35 to 44, it was 31% (+10 percentage points), for those aged 45 to 64, it was 22% (+4 percentage points), and for those aged 65 and older, it decreased slightly to 9% (-1 percentage point).
Parents of children under 18 saw a substantial increase in high stress levels, with 33% reporting this in 2023, compared to 24% in 2019.
In 2023, parents were more likely than other adults to report increased financial strain in their households (46% vs. 34%), frequent arguments about money (58% vs. 30%), and feeling overwhelmed by worries about finances (66% vs. 39%).
Alarmingly, parents of children under 18 were also more likely than other adults to report feeling completely overwhelmed by stress most days (48% vs. 26%), feeling so stressed that they become numb (42% vs. 22%), or feeling so stressed that they can’t function most days (41% vs. 20%).
“Stress affects all systems of the body, so Americans must understand the serious impacts of stress and take steps to reduce the effect of stressors in their lives. Seeking help from healthcare providers, the workplace, and support systems can prevent further health crises,” noted Evans.