Somatic Symptom Disorder (SSD) is a psychiatric condition characterized by an intense focus on physical health symptoms. This disorder can cause significant emotional distress and impair daily functioning.
What Is Somatic Symptom Disorder?
Somatic Symptom Disorder refers to any mental health disorder that manifests as physical symptoms. Although these physical symptoms may resemble those of an injury or illness, they are typically not linked to any diagnosable medical condition, medication side effects, or other mental health disorders.
Despite the absence of a clear medical cause, individuals with SSD strongly believe they are ill and require treatment. According to the American Psychiatric Association, Somatic Symptom Disorder is defined as “a person’s intense focus on bodily symptoms, such as pain, weakness, or shortness of breath, that leads to significant distress and/or functional problems.”
Those affected by SSD are often consumed by their physical symptoms, and their thoughts, emotions, and behaviors are heavily influenced by them. The symptoms are generally not intentionally fabricated or consciously produced. A diagnosis of Somatic Symptom Disorder is not made merely because there is no medical explanation for the physical symptoms. Rather, it is based on whether the individual’s thoughts, feelings, and behaviors about their condition are disproportionate. The diagnostic process may also consider the patient’s medical and family history. Treatment, which emphasizes a strong, supportive relationship between doctor and patient, can be highly effective in managing the disorder.
Understanding Somatic Symptom Disorder
Somatic Symptom Disorder (SSD), also known as somatoform disorder or somatization disorder, is a condition characterized by persistent physical complaints that are accompanied by excessive and maladaptive thoughts, emotions, and behaviors related to these symptoms. As defined by The Merck Manuals, “Somatic symptom disorder is marked by multiple ongoing physical complaints, with an exaggerated response to those symptoms that often leads to an irrational belief that the medical issues are life-threatening, even when reassured by a doctor and normal test results.”
These symptoms can affect one or more body systems, resulting in pain, gastrointestinal distress, neurological problems, and sexual symptoms. Individuals with Somatic Symptom Disorder often experience anxiety in addition to their physical complaints. According to Harvard Medical School, the person with SSD “may be reacting to ordinary bodily sensations or a mild illness,” but they tend to experience heightened anxiety and are more likely to feel threatened by health concerns than most individuals. However, as Harvard points out, the individual is not fabricating these symptoms, as the distress caused by them is real.
Common behaviors exhibited by someone with Somatic Symptom Disorder include:
- Consulting multiple healthcare providers simultaneously
- Showing little to no response to medical treatments
- Being highly sensitive to medication side effects
- Failing to feel reassured by a diagnosis or treatment
While these behaviors are common in SSD, it is important to note that individuals affected by somatoform disorders may also be dealing with serious underlying medical conditions. As a result, a thorough evaluation by a physician is essential. Doctors typically perform a range of tests to rule out other potential causes before diagnosing the disorder.
A 2017 research paper on somatization and Somatic Symptom Disorders (SSD) explains that, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Somatic Symptom and Related Disorders (SSRD) are defined as “chronic somatic symptoms linked with uncontrollable thoughts, feelings, and behaviors, regardless of whether a medical explanation for these symptoms can be identified” (Dimsdale, 2017).
Prevalence Of Somatic Symptom Disorder
A 2017 study by Dehoust et al. highlights that somatic symptom disorders, also referred to as somatoform disorders or somatization disorders, have rarely been addressed in epidemiological studies and health care assessments of the elderly. According to the study’s findings, which were derived from a survey of 3142 community-dwelling respondents aged 65–84 from six European countries using the Composite International Diagnostic Interview, the 12-month prevalence rate for any somatoform disorder was 3.8%. Notably, the prevalence for somatization disorder as per DSM-IV was found to be 0%, while abridged somatization occurred in 1.7% of respondents, and the rate for 12-month somatoform pain disorder was 2.6%.
Additional data from Harvard Health Publishing suggests that a significant portion of outpatient medical visits worldwide—ranging from one-third to one-half—are related to symptoms such as pain or fatigue with no clear physical cause. Individuals presenting with such unexplained symptoms often meet the criteria for somatoform disorders as defined by the DSM-IV. A further study by Nomura, Kuboki, and Yamanaka involving 424 outpatients provides more insights into the prevalence of somatoform disorders, revealing that among the diagnoses categorized under Axis I of DSM-IV, somatoform disorders (18.2%) ranked just below eating disorders (19.4%). Within the somatoform disorders, somatoform disorder not otherwise specified was the most common (32.5%), followed by pain disorder (22.1%), conversion disorder (19.5%), hypochondriasis (14.3%), and undifferentiated somatoform disorder (11.7%).
Somatic symptom disorder, often referred to as SSD or somatoform disorder, is a prevalent and debilitating condition among older adults. It is frequently associated with other mental health conditions, underscoring the need for further research and clinical attention to better understand and treat this disorder.
Somatic Symptom Disorder Related Conditions
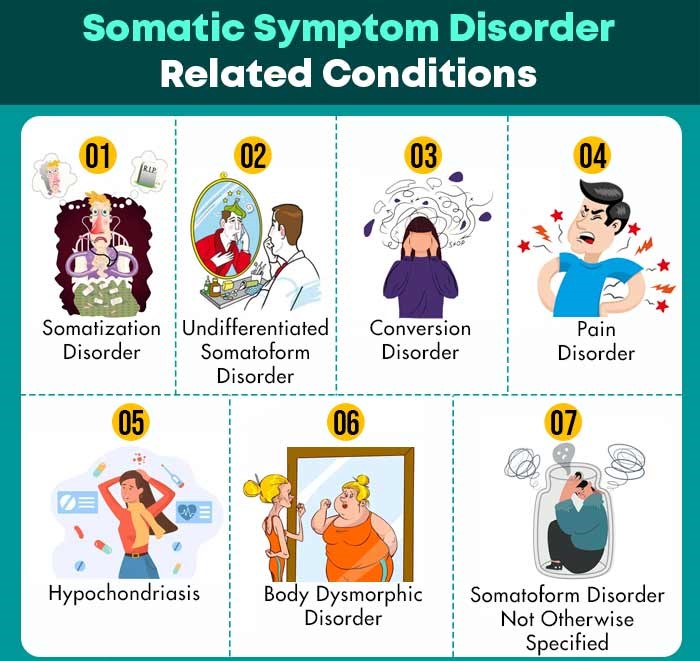
Somatic Symptom Disorder (SSD) and other related somatoform disorders are located at the extreme end of the somatization spectrum. These disorders are characterized by the prolonged persistence of severe physical symptoms, which cannot be fully explained by any physical illness. Some of the key somatoform disorders include:
- Somatization disorder
- Hypochondriasis
- Conversion disorder
- Body Dysmorphic Disorder
- Pain disorder
- Somatoform Disorder Not Otherwise Specified
These conditions are categorized as mental health disorders, as the symptoms are believed to stem from psychological factors. However, they cannot be fully explained by other recognized mental health issues, such as depression, substance abuse, or other psychiatric disorders.
1. Somatization Disorder
Individuals with Somatization Disorder experience physical symptoms that cannot be explained by any medical condition. These symptoms typically begin before the age of 30 and persist for several years. The disorder is marked by a combination of at least two gastrointestinal issues, one pseudoneurological problem, four pain-related symptoms, and one sexual symptom.
Patients with Somatization Disorder often require frequent clinical visits, numerous imaging and laboratory tests, and various referrals to explore the underlying causes of their symptoms. According to the AFP Journal, somatization disorder is more prevalent in women than men, with a lifetime prevalence ranging from 0.2% to 2% in women and 0.2% in men.
This revised version maintains the original meaning while ensuring the keyword density of “Somatic Symptom Disorder,” “SSD,” “Somatoform Disorder,” and “somatization disorder” is under 2%.
2. Undifferentiated Somatoform Disorder (SSD)
Undifferentiated somatoform disorder, also referred to as SSD, is characterized by a less-specific manifestation of somatization disorder. This condition is diagnosed when a patient reports one or more unexplained physical symptoms over a period of six months or longer, alongside other clinical criteria. Chronic fatigue is a common symptom that lacks a clear explanation. The majority of complaints are found among young women from lower socioeconomic backgrounds, although the disorder is not confined to any particular demographic.
3. Conversion Disorder
Conversion disorder involves symptoms that affect sensory functioning, leading to the assumption of a neurologic condition, which is ultimately considered pseudoneurologic. The symptoms do not align with established anatomical pathways or physiological mechanisms. However, they often reflect common lay perceptions of physiology, offering a clue to the presence of somatic symptom disorder (SSD). Patients may exhibit symptoms dramatically or show indifference to their condition. Typically, symptoms arise before the age of 10 or after 35, and this disorder is more prevalent in rural areas, individuals from lower socioeconomic backgrounds, and those with limited medical or psychological knowledge.
4. Pain Disorder
Pain disorder is relatively common and typically has psychological factors at its onset. While pain is the central feature of this disorder, psychological factors significantly influence the perception and experience of pain. Individuals with this disorder often seek frequent medical attention, use medications regularly, and may experience challenges in their personal relationships, employment, or family life. It can also lead to inactivity and social isolation, frequently occurring alongside comorbid conditions such as distress, anxiety, or substance-related disorders.
5. Hypochondriasis
Patients with hypochondriasis often misinterpret physical symptoms and develop an intense fear of having serious, life-threatening medical conditions. A key diagnostic criterion is the persistence of these concerns, which must continue for at least six months without delusion. The prevalence of hypochondriasis ranges from 2% to 7% in primary care settings, and there are no significant differences in terms of age, sex, or cultural background. The defining characteristic is the intense fear displayed by patients when discussing their symptoms, a hallmark of hypochondriasis.
6. Body Dysmorphic Disorder
Body dysmorphic disorder is characterized by an overwhelming preoccupation with a physical flaw, whether real or imagined. When a physical defect is present, it is typically minor, yet the individual’s concern is excessive. This disorder affects both men and women equally.
7. Somatoform Disorder Not Otherwise Specified
Somatoform disorder not otherwise specified (SSD) refers to a psychiatric condition where a person exhibits physical symptoms that do not fully align with the criteria for other somatoform disorders but still lead to significant distress or impairment. This condition encompasses various ailments, such as pseudocyesis, which is the mistaken belief of being pregnant, despite experiencing symptoms like abdominal enlargement, nausea, breast changes, and labor pains. These physical symptoms are often misunderstood or fabricated, leading to distress.
Symptoms Of Somatic Symptom Disorder
The exact symptoms of Somatoform Disorder (SSD) and related disorders are not fully understood. There may be issues with nerve impulses that send signals of pain, pressure, and other unpleasant sensations to the brain, but it is unclear whether these sensations are real or imagined. However, some common symptoms of Somatoform Disorder (also referred to as Somatization Disorder) include:
- Distinct sensations of pain or shortness of breath, alongside more general symptoms such as fatigue or weakness.
- Symptoms that cannot be explained by a recognized medical cause, or symptoms that may be associated with conditions like cancer or heart disease, but are more intense than expected for those conditions.
- One specific symptom, multiple symptoms, or a variety of symptoms may be present.
- Symptoms can vary in intensity, ranging from mild to moderate to severe.
Pain is the most common symptom, but regardless of the specific symptoms, excessive thoughts, feelings, or behaviors related to them can lead to significant difficulties in daily life. This may result in problems at work or, in some cases, disability.
These thoughts, emotions, and behaviors may include:
- Persistent worry about potential illness.
- Interpreting normal physical sensations as signs of severe physical illness.
- Fearing that symptoms are more serious than they actually are, even when there is no medical evidence.
- Perceiving physical sensations as frightening or harmful.
- Believing that medical exams or treatments are inadequate.
- Fearing that physical activity may cause harm to the body.
- Frequently checking for irregularities in the body.
- Seeking routine medical care that fails to alleviate concerns, or even worsens them.
- Being unresponsive to medical treatments or excessively concerned about the side effects of medications.
- Experiencing impairment that is more severe than what would typically be expected from the medical condition.
Causes Of Somatic Symptom Disorder
Somatoform disorders (SSD), also known as somatization disorder, can affect individuals across all age groups. However, determining the exact prevalence of these disorders is challenging, as many cases remain undiagnosed. The specific reasons why people develop SSD are not fully understood, but certain factors seem to increase the likelihood of developing somatoform disorders. For instance, individuals with a history of alcohol and drug abuse are more prone to these conditions. However, alcohol and drug use may influence both the cause and the effect of somatoform disorders. The causes of SSD are varied, and some of the most common include:
- A childhood upbringing where emotional expression is restricted, limiting the child’s ability to communicate feelings
- A background where abuse is prevalent, leading the child to respond with physical symptoms rather than expressing fear
- An environment where the child gains attention primarily through physical complaints
- Traumatic events in childhood or adolescence that lead to the emotional “splitting,” a coping mechanism to manage normal life
- Traumatic experiences in adulthood that may trigger the onset of somatoform disorders
- Genetic factors that can contribute to the development of SSD. Genetic makeup refers to the inherited traits from one’s parents that influence various bodily functions. This genetic predisposition, in combination with other factors such as upbringing style, family relationships, and peer connections, can play a role in the development of somatoform disorders.
This expanded view of SSD highlights the multiple factors that can contribute to its onset, from environmental and emotional influences to genetic predispositions.
Diagnosis Of Somatic Symptom Disorder
The diagnosis of somatic symptom disorder (SSD), also known as somatization disorder, can often cause significant stress and frustration for patients. They might feel upset if there is no clear physical evidence supporting their symptoms or if they are told that their concern about a physical illness is disproportionate.
However, diagnosing somatic symptom disorder (SSD) and related conditions can be challenging. The healthcare provider will typically perform a physical exam and may conduct additional tests. If the results indicate that there is no underlying physical illness, the doctor might refer the patient to a mental health professional for further evaluation and support.
Treatment Of Somatic Symptom Disorder
Patients experiencing unexplained physical symptoms often believe their symptoms have a physical origin, even though the underlying cause may not be physical. These beliefs are based on a misunderstanding of the symptoms themselves. However, effective treatment for somatoform disorders, including Somatic Symptom Disorder (SSD) and somatization disorder, is available. The following steps outline the approach to treatment:
1. Discussing the Diagnosis
The first step in treating somatoform disorders is to have a conversation with the patient about the possibility of such a disorder. This discussion comes after ruling out organic causes as the primary explanation for the symptoms, confirming a psychiatric diagnosis. A psychiatric diagnosis should only be made once all necessary criteria have been met.
Explaining the diagnosis requires careful planning and preparation. The physician must establish a therapeutic relationship with the patient, which involves acknowledging the discomfort associated with the unexplained physical symptoms. Compassion and understanding should be maintained throughout the process.
2. Therapy Treatment
Once the diagnosis is confirmed and accepted by the patient, the physician may begin addressing any psychiatric comorbidities. It is important to note that psychiatric disorders rarely occur in isolation, and somatoform disorders like SSD and somatization disorder are no exception. Conditions such as clinically significant depression, personality disorders, anxiety disorders, and substance abuse may frequently coexist with somatoform disorders. These should be treated simultaneously using appropriate methods.
Cognitive Behavioral Therapy (CBT) has proven effective in treating SSD and other somatoform disorders. CBT targets cognitive distortions, irrational beliefs, excessive worry, and behaviors that contribute to health anxiety and somatic symptoms. The benefits of CBT include a reduction in the frequency and severity of symptoms, lower healthcare costs, and improved overall patient functioning【mfn]Kleinstäuber, M., & Rief, W. (2017). Cognitive behavioral therapy for somatoform disorders and pain. The Science of Cognitive Behavioral Therapy, 405-427. https://doi.org/10.1016/b978-0-12-803457-6.00017-9[/mfn].
Read More About Cognitive Behavioral Therapy (CBT) Here
3. Medications
Antidepressants are commonly prescribed to patients diagnosed with somatoform disorders (SSD). However, the exact mechanism by which antidepressants aid those with SSD remains unclear. These medications may help indirectly by alleviating symptoms associated with depression, anxiety, or post-traumatic stress disorder, which are frequently observed in individuals with somatoform disorders. Additionally, antidepressants might have a direct impact on nerve circuits, influencing not only mood but also symptoms such as fatigue, pain perception, gastrointestinal issues, and other complaints common in patients with somatization disorder.
4. Follow-Up
Regular follow-up appointments with a healthcare provider are essential for patients with somatoform disorders. These visits help maintain a strong therapeutic relationship and foster an atmosphere of trust and support. They give patients the opportunity to express concerns related to their condition and receive reassurance that their symptoms are not indicative of a physical illness. Consistent follow-up visits also help prevent unnecessary healthcare visits and reduce the risk of excessive treatments, ensuring that patients receive the most appropriate care for their condition.
How To Help Someone With Somatic Symptom Disorder
When physical symptoms typically associated with somatoform disorders, such as SSD (Somatoform Disorder) or somatization disorder, are ruled out, it can be difficult for patients to accept that a potentially life-threatening illness has been eliminated as the cause. These physical symptoms can create significant distress for the individual, and reassurance alone may not always provide relief.
It is important to encourage your loved one to consider the possibility of a mental health condition and to explore strategies for managing the symptoms. Physical disability may lead the person to feel helpless, requiring additional physical care and emotional support. This burden can be overwhelming for the caregiver, creating stress within the family and impacting other relationships.
Self-help Strategies For Somatic Symptom Disorder
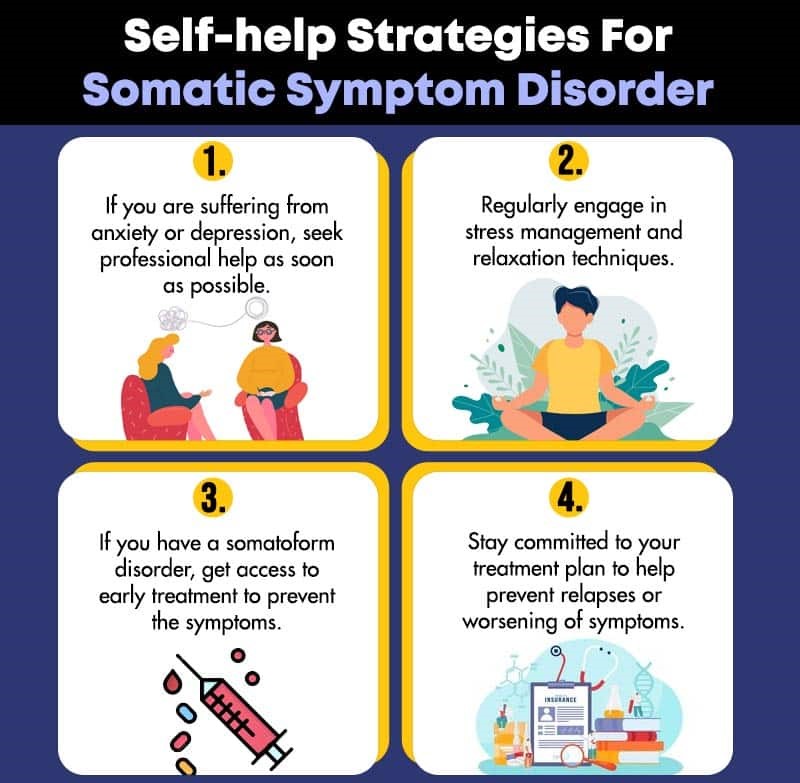
There is limited information available regarding self-care for individuals with somatic symptom disorder (SSD). Nevertheless, the following suggestions may be beneficial.
If you are dealing with anxiety or depression, it is important to seek professional assistance promptly.
Recognize the signs of stress and how it impacts your body. Make a habit of practicing stress management and relaxation techniques regularly.
If you suspect that you may have a somatoform disorder or somatization disorder, seek early treatment to avoid the worsening of symptoms and to preserve your quality of life.
Remain dedicated to your treatment plan to help reduce the likelihood of relapses or the intensification of symptoms.
Risks And Complications Of Somatic Symptom Disorder

Somatoform Disorder (SSD) is linked to various risks and complications, including several risk factors. These include:
Risk Factors
- Experiencing symptoms of anxiety or depression
- Having an existing medical condition or recovering from one
- Being at higher risk for developing a medical condition, particularly if there is a strong family history of a specific disease
- Dealing with high levels of stress due to life events, trauma, or violence
- Experiencing past traumatic events, such as childhood sexual abuse
- Having a lower level of literacy or being in a disadvantaged socio-economic status
These factors play a significant role in the development and progression of somatization disorder and should be closely monitored in individuals affected by SSD.
Read More About Anxiety Here
Complications
- Decline in overall health
- Impaired daily functioning, which may include physical disability
- Strained relationships with family, friends, and colleagues
- Struggles with employment or potential unemployment
- Co-occurring mental health issues, such as anxiety, depression, and personality disorders
- Increased suicidal thoughts associated with depression
- Financial strain due to frequent and unnecessary healthcare visits related to somatization disorder or SSD
Read More About Major Depressive Disorder Here
Is Somatic Symptom Disorder Completely Curable?
Treating individuals with Somatoform Disorder (SSD), also known as somatization disorder, presents numerous challenges. It requires considerable time, patience, and compassion. Before confirming a diagnosis of somatoform disorder, it is essential to rule out any organic medical conditions and address potential psychiatric concerns. Once these factors are excluded, a well-structured care plan should be developed to help the patient recognize the disorder and feel comfortable discussing their concerns openly. Additionally, continuous support from family and loved ones plays a crucial role in assisting the patient in managing and coping with this condition effectively.
Somatic Symptom Disorder At A Glance
- Somatic symptom disorder (SSD) refers to any mental health condition that is expressed through physical symptoms.
- This disorder is also referred to as somatoform disorder or somatization disorder.
- Somatic symptom disorder is a prevalent condition and is recognized as a highly debilitating issue, particularly in older adults.
- The process of diagnosing somatic symptom disorder can cause significant stress and frustration for those affected.
- Effective treatment for individuals with somatic symptom disorder is challenging, time-consuming, and demands persistence and a compassionate approach.