Shared Psychotic Disorder (SPD), also referred to as Folie à Deux, is a rare mental condition in which one or more individuals without mental health issues develop delusions after being closely associated with someone who has a psychotic disorder. The term Folie à Deux translates to “madness shared by two.”
What Is Shared Psychotic Disorder?
Shared Psychotic Disorder (SPD) is an unusual psychiatric disorder where a delusion is shared between two or more people with strong emotional bonds. In SPD, a mentally healthy person begins to adopt the delusions and, in some cases, hallucinations of someone suffering from a psychotic disorder. SPD is also known by other terms such as shared delusional disorder (SDD) or shared psychosis. According to a 2010 study, “Shared psychotic disorder (folie à deux) is a rare disorder characterized by delusions and demonstrates intercultural differences.”
Typically, SPD is seen in individuals who are in close personal relationships, such as family members. In this scenario, a mentally healthy person (the secondary or acceptor) begins to believe the delusions of another individual who has a psychotic or delusional disorder (the primary or inducer). This condition is most common among family members, such as sisters, parents and children, or spouses. The Merck Manuals explain that “The patient with the primary disorder is usually the socially dominant member in the relationship and imposes the delusion on or convinces the patient with the secondary disorder of the unusual beliefs.”
In order to properly diagnose and treat SPD, it is crucial to identify the inducer—the person with the primary psychosis. The secondary individual typically abandons the delusional beliefs once they are separated from the inducer, making early intervention important for effective treatment.
Origins Of Folie à Deux
Shared Psychotic Disorder (SPD) was first documented in 1860 by Baillarger. However, the disorder was more formally conceptualized in 1877 by Charles Lasègue and Jean-Pierre Falret, who referred to it as Folie à Deux. This condition was also commonly known as Lasègue-Falret syndrome (Arnone, D., Patel, A., & Tan, G. M., 2006).
SPD refers to a group of disorders in which symptoms, such as paranoid delusions, are transferred from one individual to one or more people who are closely connected. During the 19th century, the disorder was recognized under various other terms, including Folie communique or communicated psychosis in France, and Induziertes Irresein in Germany, a term introduced by Lehman and Sharfetter.
The transfer and sharing of delusional beliefs is referred to as Folie à Deux when it occurs between two individuals, Folie à Trois when three individuals are involved, and Folie à Quatre when four individuals are affected. When an entire family is involved, it is termed Folie en famille or “family madness” (Jolfaei, A. G., Isfahani, M. N., & Bidaki, R., 2011). However, when a group or community shares a delusion, like in cults, it is called Folie à Plusieurs or “madness of several.” For example, if a cult leader experiences a psychotic disorder and holds delusional beliefs, it is likely that the followers will also adopt those delusions, as seen in the Heaven’s Gate mass suicide.
SPD was initially listed as “shared paranoid disorder” in DSM-III but was later reclassified as shared psychotic disorder in DSM-IV. In ICD-10, it was termed induced delusional disorder. In the latest version, DSM-5, this condition is now categorized under “other specified schizophrenia spectrum and other psychotic disorders.” The DSM-5 states that all individuals affected by SPD are diagnosed with a “delusional disorder,” without distinguishing between the primary and secondary cases for diagnostic purposes. However, making such distinctions could be important for treatment.
Understanding Shared Psychotic Disorder
Shared Psychotic Disorder, also referred to as Folie à Deux, psychosis by association, and induced psychotic disorder, is a rare and distinctive psychiatric condition, as noted in a 2011 scientific review by Christensen and Ramos. Individuals affected by Shared Psychotic Disorder may experience a loss of contact with reality and often struggle with daily functioning. The condition is primarily characterized by delusions and hallucinations, where sufferers perceive unreal events and believe in false notions, even when confronted with evidence contradicting their beliefs.
This disorder typically arises in individuals who share a close, long-term relationship, where one person assumes a dominant role while the other remains passive. Often, the individuals involved are related by blood or marriage. The delusional beliefs of the dominant person influence the secondary individual, and these delusions may subside or disappear if the relationship is disrupted or if the individuals are no longer in close contact.
While those suffering from Shared Psychotic Disorder may exhibit strong emotional bonds with each other, they often lack broader social connections. Although the precise cause of the disorder is not fully understood, researchers suggest that social isolation and stress might play significant roles. Studies indicate that Shared Psychotic Disorder tends to develop in individuals who are predisposed to psychosis, especially in environments marked by social isolation and an association with someone already experiencing psychotic symptoms.
In family settings, it is common for one parent to act as the primary individual, with children adopting the parent’s delusional beliefs to varying extents. This can lead to the children developing irrational beliefs, such as conspiracies involving alien abductions or government surveillance. Unfortunately, individuals with this condition rarely seek treatment, and the disorder is typically identified when the primary individual seeks help, or when the secondary person begins to exhibit signs of the delusion.
Prevalence Of Shared Psychotic Disorder
The prevalence of Shared Psychotic Disorder (SPD), also known as Folie à Deux, remains unclear, though it is generally regarded as a rare condition. However, some studies suggest that between 1.7% and 2.6% of psychiatric hospital admissions are affected by SPD. These figures may be inaccurate, as the condition is often under-diagnosed.
Additionally, many individuals with Shared Psychotic Disorder do not seek treatment, primarily because they are unaware of their mental illness. This lack of awareness leads some experts to believe that SPD may be more common than it is typically perceived to be. It has also been observed that women, particularly those with delusional dominant partners, are more likely than men to develop SPD.
A 2012 research paper noted that Folie à Deux, also known as communicated insanity, contagious insanity, infectious insanity, psychosis of association, and induced psychosis, affects about 90% of nuclear families, with sister-sister relationships being the most frequently observed dyad. Treatment, including therapy and medication, can be effective in helping individuals recover from the disorder.
Types Of Shared Psychotic Disorder
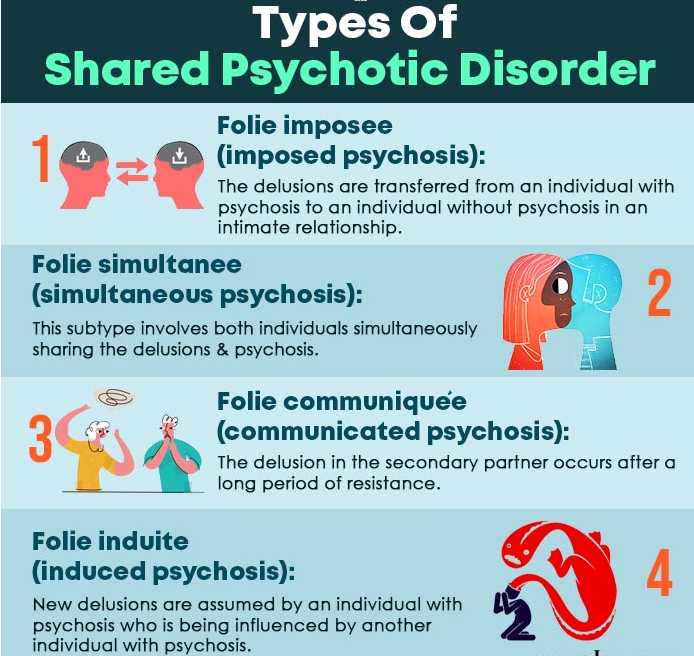
Various subtypes of Shared Psychotic Disorder (SPD) have been identified, each with distinct characteristics. These include:
- Folie imposee (imposed psychosis)
First conceptualized in 1877 by Lasègue and Falret, this subtype refers to the transfer of delusions from one individual to another within an intimate relationship. In this scenario, the dominant person exhibits persecutory delusions, while the secondary individual is suggestible and submissive. These delusions tend to diminish or disappear when the two people are separated. - Folie simultanee (simultaneous psychosis)
Described by Regis in 1880, this subtype involves both individuals simultaneously sharing delusions and psychosis. Research suggests a possible genetic predisposition for this condition, especially among family members and siblings. Furthermore, prolonged social isolation is also considered a contributing risk factor. - Folie communiquée (communicated psychosis)
This subtype was originally detailed in 1881 by Marandon de Montyel and closely resembles Folie imposee (imposed psychosis). However, in Folie communiquée, the second individual initially resists the delusions of the primary individual. Over time, they may succumb to the delusional beliefs, even maintaining them after separation from the primary case. - Folie induite (induced psychosis)
Described by Lehmann in 1885, this subtype occurs when the second individual adopts additional delusions that are introduced by the primary partner. In this case of Shared Psychotic Disorder, the delusions often expand, and the condition is typically observed in individuals both suffering from mental illnesses.
Each of these subtypes highlights the complexity and varying dynamics of Shared Psychotic Disorder, also known as Folie à Deux.
Shared Psychotic Disorder And Delusions
The severity of Shared Psychotic Disorder (SPD), also known as Folie à Deux, and its symptoms largely depend on the type of delusion shared by two or more individuals. Delusions may be categorized into four major types, each with distinct characteristics:
- Bizarre delusions
These are beliefs that are physically impossible and often seen as implausible by most people within the same cultural context. An example of a bizarre delusion could be the belief that one has been abducted by aliens and is being operated on or experimented upon. - Non-bizarre delusions
This type includes delusional beliefs that, while possible, are highly improbable and can be understood by people from the same culture. For instance, someone with this type of delusion may believe that the FBI is tracking their smartphone and constantly monitoring them, which, although conceivable, is extremely unlikely. - Mood-congruent delusions
These delusions align with the person’s emotional state, whether manic or depressed, during a particular time. For example, during a manic episode, a person may believe they are destined to win the lottery or strike it rich at a casino, despite no logical reason to think so. Conversely, in a depressive state, they may believe that they or a loved one will die in an accident, even without any supporting evidence. - Mood-neutral delusions
These delusions are not influenced by mood and can be either bizarre or non-bizarre. They are not directly tied to the individual’s emotional state. An example could be a person believing that a family member or friend has been replaced by an imposter or doppelgänger, a belief that persists regardless of any emotional shifts.
Understanding these different types of delusions is critical in diagnosing and treating Shared Psychotic Disorder (SPD), ensuring a comprehensive approach to care and intervention.
Symptoms Of Shared Psychotic Disorder
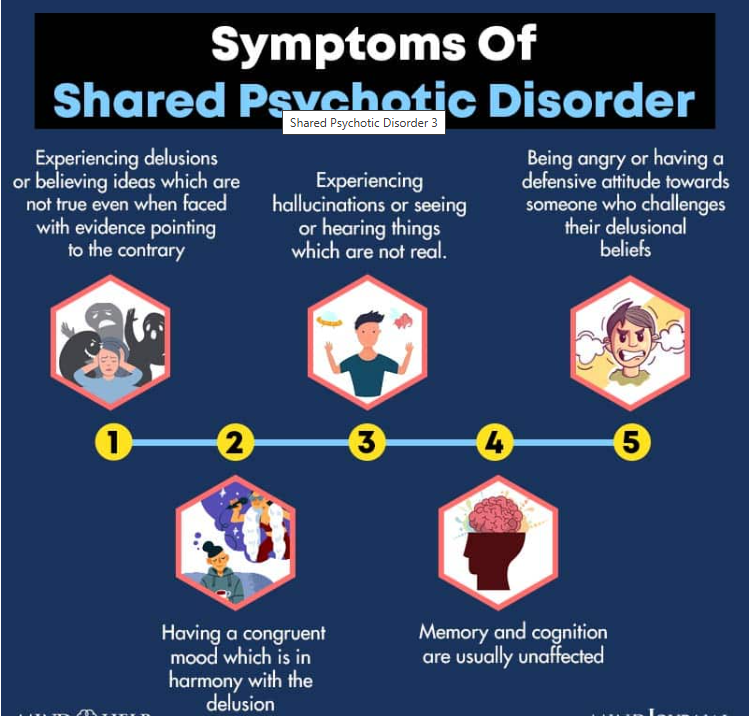
A Shared Psychotic Disorder (SPD), also known as Folie à Deux, occurs when an individual develops a shared delusion while in a close relationship with someone who already has an established delusion. Below are some common symptoms associated with SPD:
- Believing in delusions or ideas that are false, despite clear evidence to the contrary.
- Experiencing hallucinations, such as seeing or hearing things that aren’t real; the secondary partner may also experience hallucinations.
- Displaying anger or defensiveness when their delusional beliefs are questioned or challenged.
- Demonstrating relevant and coherent speech.
- Exhibiting a mood that aligns with the delusion, maintaining emotional congruence.
- Having structured, goal-directed thoughts while sharing delusional ideas.
- Less likely to show signs of distorted or abnormal perceptions.
- Memory and cognitive functions generally remain unaffected.
- Typically unaware of their mental illness.
- Homicidal or suicidal thoughts and behavior may sometimes occur.
- Both the primary individual and the secondary partner may appear outwardly normal, well-groomed, and appropriately dressed.
This description highlights the key signs of Shared Psychotic Disorder (SPD), also referred to as Folie à Deux, and emphasizes how both individuals involved may show similar symptoms despite being unaware of the disorder.
Read More About Anger Here
Causes Of Shared Psychotic Disorder

The precise causes of Shared Psychotic Disorder (SPD), also known as Folie à Deux, remain unclear, but there are several risk factors that have been linked to the condition. These factors include:
Age
The age of the partners can also play a crucial role in the development of SPD. Research has indicated that an age gap between the primary and secondary partners may cause the older individual to be more dominant, while the younger partner may become more submissive. Studies have suggested this dynamic as a potential risk factor for the development of Folie à Deux and Shared Psychotic Disorder【mfn] Shimizu, M., Kubota, Y., Toichi, M., & Baba, H. (2007). Folie à deux and shared psychotic disorder. Current psychiatry reports, 9(3), 200–205. https://doi.org/10.1007/s11920-007-0019-5 [/mfn].
Untreated Mental Illness in the Primary Partner
Chronic mental illnesses can have severe consequences when left untreated, often leading to significant social problems that affect the lives of those around the person. In cases of SPD, the primary partner is typically dealing with delusional disorder, schizophrenia, or an affective disorder, which can influence the secondary partner’s mental health.
Read More About Aging Here
3. Gender
It has been observed that gender plays a significant role in Shared Psychotic Disorder (SPD), with this condition being more commonly seen in women. This occurs not only in the secondary partner but also in the primary case, where women are more frequently affected by Folie à Deux.
Read More About Gender Here
4. Type of Relationship
Research on Shared Psychotic Disorder (SPD), also known as Folie à Deux, indicates that the disorder typically develops among family members. The most common relationships observed between the primary and secondary individuals are married or common-law couples, with sisters being the second most common pairing.
5. Duration of the Relationship
Studies suggest that the length of the relationship is a crucial factor in the development of SPD. The emotional attachment that the secondary partner has with the primary individual significantly influences their adoption of delusional beliefs.
6. Social Isolation
Social withdrawal and isolation are prevalent in many cases of SPD. A lack of social interaction can make the secondary partner more susceptible and suggestible to the primary partner’s influence. Without social comparison, they may become easily manipulated under stressful or fearful circumstances. To maintain their connection, the secondary partner may adopt the primary individual’s beliefs, eventually coming to accept them as truth.
7. Cognitive Impairment
Experts note that the secondary partner in Folie à Deux often demonstrates limited intelligence and poor judgment, which can contribute to their susceptibility to the delusions of the primary case.
8. Personality Issues
Personality factors can also significantly contribute to Shared Psychotic Disorder. Secondary individuals are often emotionally immature, introverted, and neurotic. Research has shown that premorbid personality traits such as dependency, schizotypal tendencies, or schizoid behavior can play a major role in the onset of SPD.
9. Communication Problems
Problems in communication can hinder the exchange of ideas and emotions, leading to social withdrawal and isolation. Experts believe that improving communication within dyadic relationships could help both individuals view differing perspectives, potentially alleviating rigid and mindless thinking. This can be achieved through conjoint psychotherapy, as suggested in case studies on Folie à Deux.
10. Comorbidity of the Secondary Partner
Research indicates that secondary individuals who have been diagnosed with significant mental health disorders, such as dementia, bipolar disorder, depression, mental retardation, or schizophrenia, are more vulnerable to being influenced by someone with similar or related mental health issues, thus increasing the likelihood of developing SPD.
11. Stressful Life Events
Negative life events can profoundly affect an individual’s mindset and behavior, leading them to adopt specific delusions. These stressful events can influence the relationship between the primary and secondary individuals, diminishing the secondary partner’s ability to resist the delusional beliefs and emotions imposed by the primary person in Folie à Deux.
Diagnosis Of Shared Psychotic Disorder
Shared Psychotic Disorder (SPD), also known as Folie à Deux, is not recognized as a distinct diagnosis in the latest DSM-5. Instead, it is categorized under “Other specific schizophrenia spectrum and other psychotic disorders.” Diagnosing SPD is challenging, as the secondary partner typically does not seek professional help.
The secondary individual is often unaware that their delusions and distorted beliefs have been influenced by a dominant person they are emotionally close to. Because these delusions are adopted gradually, the secondary person’s resistance and skepticism tend to diminish over time.
To be diagnosed with SPD, a person must meet certain criteria:
- The condition must involve a delusion acquired through a close personal relationship between the primary and secondary individuals. The primary individual must already have an established delusion.
- The delusional beliefs of the secondary person must mirror or resemble the primary individual’s delusion.
- The delusion must not be caused by another mental illness, such as a psychological or mood disorder, a general medical condition, medications, or substance abuse.
As with most psychiatric conditions, no specific laboratory tests are required to diagnose SPD. However, brain imaging, blood tests, or physical exams may be used to rule out other medical causes. Mental health professionals, including psychiatrists, psychologists, or doctors, may ask questions to gather the medical and psychiatric histories of both the primary and secondary individuals.
Once other causes have been excluded, the doctor may conduct a clinical interview to evaluate the patient’s behavior and attitudes. A mental state examination may also be performed, and a third party may be consulted to help further understand the condition.
Complications Of Shared Psychotic Disorder
If left untreated, Shared Psychotic Disorder (SPD), also known as Folie à Deux, can evolve into a chronic condition. It may lead to symptoms such as aggression, depression, anxiety, and complete social withdrawal. Furthermore, patients with SPD may develop suicidal or homicidal tendencies when they begin to act on their delusional thoughts and beliefs. A 2013 study (Guivarch, J., Piercecchi-Marti, M. D., & Poinso, F., 2018) of SPD cases revealed that “homicides were committed with significant violence, typically directed at a family member, and were sometimes followed by suicide.”
The study suggests that a combination of persecutory and mystical delusions was a major contributing factor for homicide in these cases. It also noted that “the homicides occurred in response to destabilization of the delusional dyads.” By acting on their paranoid delusions, individuals with SPD may inadvertently commit violent acts, endangering both their own lives and the lives of others.
Treatment Of Shared Psychotic Disorder
Standard treatment methods for Shared Psychotic Disorder (SPD), also known as Folie à Deux, are not well-established due to the rarity of the condition. Additionally, it is often undiagnosed and left untreated. While the primary individual may receive treatment, the secondary partner often remains unidentified, and thus untreated. However, once the secondary sufferer is recognized, various treatment approaches can be employed to help alleviate the symptoms of SPD and reduce the delusions associated with it.
As noted in Unusual Psychiatric Syndromes by Bhandari, S. (2012), published in Core Psychiatry (Third Edition), the initial step in managing Folie à Deux is to separate the two individuals affected by the delusions. This is crucial, as approximately 40% of secondary sufferers show positive responses to this intervention. Primary cases typically require therapy targeting the underlying condition, often schizophrenia, while secondary cases may need antipsychotic medication if they do not improve after separation. Additionally, addressing the issue of social isolation is critical, and family therapy, along with strong social support, can play a significant role in helping individuals overcome their delusions.
The following treatment options are available for managing the symptoms of shared psychotic disorder (SPD):
1. Therapy
Therapeutic interventions are commonly used to treat SPD. The most effective types of therapy for SPD include:
- Psychotherapy
- Family therapy
Let’s explore how these therapeutic practices can aid in the recovery from this disorder:
A. Psychotherapy
Psychotherapy is a proven psychological intervention that addresses a wide array of psychological, behavioral, and physical concerns, making it a fundamental treatment approach for mental and somatic disorders. A 2019 study highlights psychotherapy’s role in managing various conditions, including SPD, stating that it is an essential treatment for health care management (Locher, C., Meier, S., & Gaab, J., 2019). Individual psychotherapy, through one-on-one counseling, is designed to reduce anxiety and stress while helping the patient recognize their distorted thinking and behavior patterns. As the therapist establishes trust, they can engage the patient in deeper conversations about their mindset and assist them in understanding their issues better.
Over time, therapy can help patients identify delusions and promote healthier thinking patterns. Although it may be difficult, particularly since the sufferer may not recognize their condition, psychotherapy helps alleviate emotional distress and assists in separating the secondary person from the primary individual with the original delusions.
B. Family Therapy
Family therapy, as outlined in a 2020 study, is another key intervention. It promotes the development of healthy social connections and encourages the secondary individual to explore interests outside of the shared psychosis dyad. Family therapy is designed to involve the entire family, allowing each member to improve their relationships and understand one another better. This type of therapy also works to reduce delusional thoughts within the family dynamic. Healthy family support is crucial in helping the secondary individual break free from the influence of the primary case, facilitating recovery from SPD. Additionally, it aids in building new social ties, setting life goals, following medication plans, and leading a healthier lifestyle.
2. Medications
If separating the secondary person from the primary case with the original delusions proves ineffective, medications may be prescribed for a temporary period. These medications are particularly useful for managing severe symptoms such as anxiety, insomnia, and restlessness. Common medications prescribed for shared psychotic disorder include:
- Antipsychotics
- Antidepressants
- Mood stabilizers
- Tranquilizers
- Sedatives
Antipsychotics are effective in managing delusions and hallucinations, which are often associated with psychosis. However, they may not provide a cure for psychosis. Research indicates that the use of medications, such as antipsychotics, antidepressants, and mood stabilizers, can improve conditions in both primary and secondary partners affected by SPD (Arnone, D., Patel, A., & Tan, G. M., 2006).
Read More About Antidepressants Here
Coping With Shared Psychotic Disorder
“Although Shared Psychotic Disorder (SPD), also known as Folie à Deux, cannot be prevented, effective diagnosis and treatment are essential for recovery. Alongside professional intervention, there are steps individuals can take to manage and overcome the disorder. Here are a few things to keep in mind if you are recovering from SPD:
It is important to strictly adhere to your doctor’s instructions and follow the prescribed treatment plan. Consistency plays a key role in the healing process.
Continue seeing your doctor or therapist until a trusting and professional relationship is established. This connection is vital for successful treatment, even though it may feel challenging at the start.
If you or someone you know is experiencing SPD, it is crucial to seek professional help. Without treatment, this disorder can become chronic and cause further harm.
While distinguishing delusions from reality may be difficult initially, with the right treatment, a full recovery is possible. If you are the secondary individual in the relationship, it is important to work through the dependency and regain your independence.” the mentally ill primary partner and encourage them to seek help as well.
Recovery Is Possible
Shared Psychotic Disorder (SPD), also known as Folie à Deux, can be an intense, unsettling, and terrifying experience for those affected. However, it is possible to significantly reduce, or even eliminate, the symptoms with proper treatment. If you are the primary partner undergoing treatment, it is essential to communicate with your doctor about how the condition is impacting you. This allows the healthcare provider to identify the secondary person(s) involved, ensuring they also receive the necessary treatment for the shared delusion. If the secondary person is a child or otherwise unable to seek help, intervention from family, friends, or a third party is crucial to facilitate the necessary support.
With effective and appropriate treatment, it is possible not only to reduce the symptoms of Shared Psychotic Disorder but also to enable a full recovery for most patients.
Shared Psychotic Disorder At A Glance
- Shared Psychotic Disorder (SPD) is a rare psychiatric condition in which a delusion is shared by two or more individuals who have strong emotional connections.
- Shared Psychotic Disorder, also referred to as Folie à Deux, psychosis by association, or induced psychotic disorder, is an uncommon and distinct psychiatric disorder.
- The intensity of the condition and its symptoms largely depend on the type of delusion that is shared by the individuals involved.
- Although SPD cannot be prevented, a timely diagnosis and effective treatment can significantly aid in the recovery process for those affected.
- Shared Psychotic Disorder can be a deeply unsettling and frightening experience for those involved.